How climate change and nature loss are connected to the way we breathe
COPD | 12 March 2025
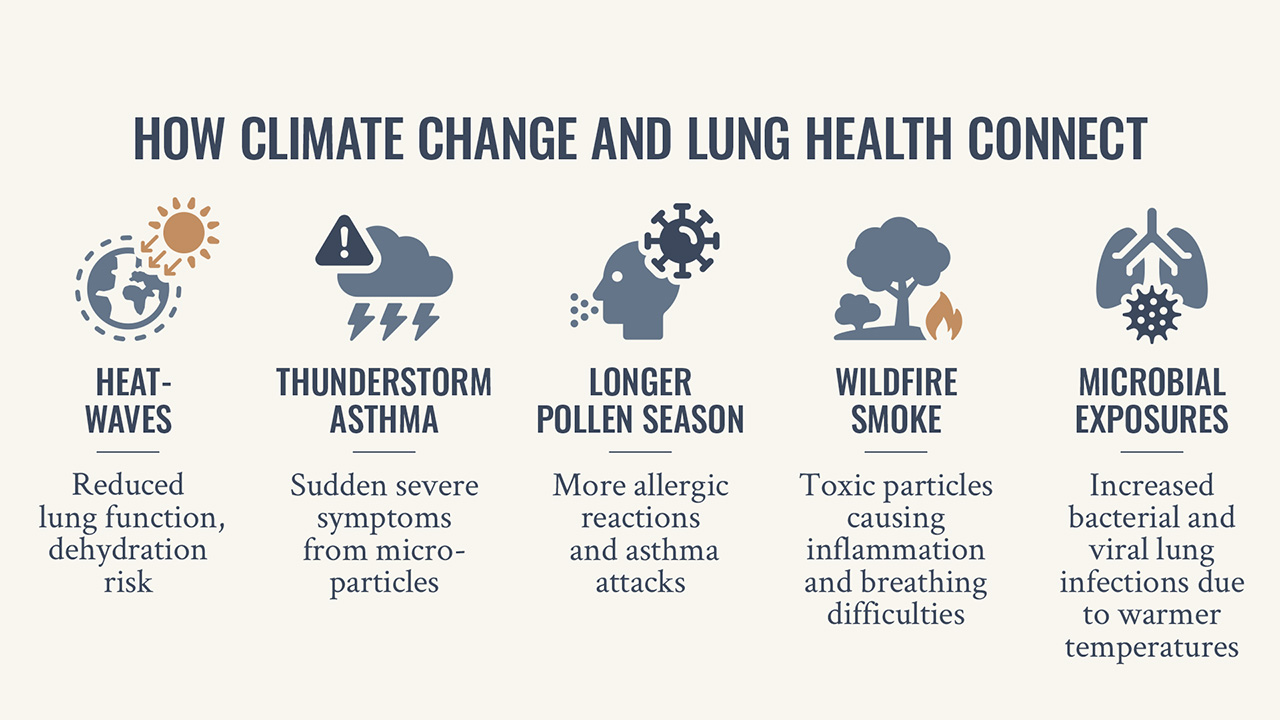
While the climate crisis often feels like a distant problem, its impacts can be as close as the air we breathe. Research1 reveals links between climate change – rising global temperatures from increased greenhouse emissions – and the daily challenges of living with asthma or COPD. There is also evidence that climate-driven events affect lung health. For example, wildfires release harmful particles that can worsen air quality2.
“Climate change is directly linked to respiratory health through events like wildfires, which increase particulate pollution and can trigger asthma and breathing difficulties,” says Dr. Tari Haahtela, Professor Emeritus of Clinical Allergology at the University of Helsinki. For those already living with asthma or COPD, it is important to be aware of how climate change can exacerbate their condition.
Rising respiratory risks
As average global temperatures continue to rise each year, a growing body of research predicts a corresponding rise in respiratory disease and cases of asthma and COPD.
“We are already seeing the effects of a warming climate on respiratory health, and the risks will only continue to grow,” Haahtela warns.
A 2013 study3 looking at the growing impact of climate change on respiratory health concluded that climate change affects lung health directly through the impact of extreme weather events, and indirectly, by changes in allergen levels, longer allergen seasons, worsened air quality and an increase in viral infections like the flu.
The study also predicted that people already with chronic respiratory disease were among those most susceptible to the adverse effects of climate change, with increased risks of exacerbations such as coughing, wheezing, breathing difficulties, emergency room visits or hospitalisations.
In 2023, a report from the Environmental Protection Agency (EPA) predicted that climate-driven warming since pre-industrial levels is projected to increase childhood asthma cases in the United States. For example, at 2°C and 4°C of warming, annual cases of asthma are expected to increase between 4% and 11%. The Global Asthma Report 20224 highlights the urgent need to mitigate these risks and act for lung health.

Heatwaves add a new layer of risk
The World Meteorological Organization (WMO) has reported that the last eight years have been the hottest on record, with heatwaves becoming more frequent and intense. Extreme heat doesn’t just make the air feel heavy and suffocating. For people with respiratory conditions like asthma or COPD, it puts extra strain on the body.
“In heatwaves, your body’s ability to regulate temperature becomes overwhelmed, especially if your respiratory system is already compromised,” Haahtela explains, drawing a comparison with taking a sauna.
While many people enjoy sitting in saunas at temperatures of over 80°C for ten-minute stints, those with respiratory issues can find this level of heat unbearable after just a few minutes.
“People with chronic respiratory diseases can’t endure the same high temperatures as those with healthy lungs. They need to step out sooner,” Haahtela says. “This is in much the same way as they struggle during heatwaves if they can’t get access to cooler spaces.”
Longer pollen seasons and surprise threats
Longer and more intense pollen seasons are worsening symptoms for people with seasonal allergies and allergic asthma. In Finland, Haahtela has seen for himself that the birch pollen season now starts one to two weeks earlier and lasts longer than it did 15 years ago.
“For people allergic to birch or grass pollen, this means an extended period of suffering,” Haahtela says.
In extreme cases, climate change also brings rare phenomena like “thunderstorm asthma,” where storms shatter pollen grains into tiny particles that strong winds carry deep into the lungs. This can cause sudden and severe asthma attacks, even in people without a history of asthma.
“Thunderstorm asthma5 is an extreme manifestation of air pollution during specific weather events,” Haahtela says, noting how desertification, also a result of climate change, in regions like the Sahara is worsening these events, especially in Mediterranean countries.
Why nature matters to our lungs
Climate change driving extreme weather events is not the only strain on our lungs. Research also ties respiratory disease to a deeper issue, our separation from nature. According to the UN, 70% of the world’s population is expected to live in cities by 2050.
This disconnection from wider nature is impacting our lung health, and, according to Haahtela, can be clearly linked6 to a rise in asthma and allergy cases.
“Our separation from wider nature lowers our exposure to diverse microbes and biogenic chemicals (what we breathe, eat, drink and touch), and disrupts our immune tolerance,” Haahtela says, “making it harder for our bodies to distinguish between harmless substances, like pollen or pet hair, from actual threats.”
“Living closer to nature and taking natural elements back to our urban life strengthens the immune system, reducing the risk of harmful inflammatory responses that lead to conditions like asthma and allergies.
So, one way to protect lung health from the worsening impacts of climate change and accelerating nature loss may lie in our relationship with nature. Haahtela points out that recognising this close link between our well-being and the planet’s health gives us even more reasons to protect it.
“By reconnecting with wider nature and making thoughtful choices in life, we don’t just protect our lungs; we strengthen our bond with the planet that sustains us.”

Dr. Tari Haahtela is a Finnish pulmonologist and allergologist, renowned for his research on asthma and allergies. He served as the Head of the Skin and Allergy Hospital in Helsinki for over 20 years and is a Professor Emeritus at the University of Helsinki. Professor Haahtela also led the influential Finnish Asthma and Allergy Programs. His research has focused on the connection between the rise of asthma and allergies and changes in environmental factors and human lifestyles.
REFERENCES
- Andersen ZJ, Vicedo-Cabrera AM, Hoffmann B, et al. Climate change and respiratory disease: clinical guidance for healthcare professionals. Breathe. 2023;19:220222. https://breathe.ersjournals.com/content/19/2/220222
- Wilgus ML, Merchant M. Clearing the air: Understanding the impact of wildfire smoke on asthma and COPD. Healthcare (Basel). 2024 Jan 25;12(3):307. doi: 10.3390/healthcare12030307. PMID: 38338192; PMCID: PMC10855577. https://pubmed.ncbi.nlm.nih.gov/38338192/
- Barnes C, Alexis NE, Bernstein JA, Cohn JR, Demain JG, Horner E, Levetin E, Nei A, Phipatanakul W. Climate change and our environment: The effect on respiratory and allergic disease. J Allergy Clin Immunol Pract. 2013 Mar;1(2):137-41. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3654689/
- Global Asthma Report 2022. https://www.globalasthmareport.org/
- Kevat A. Thunderstorm asthma: Looking back and looking forward. J Asthma Allergy. 2020;13:293-299. https://doi.org/10.2147/JAA.S265697
- Haahtela T, Laatikainen T, von Hertzen L, et al. A short history from Karelia study to biodiversity and public health interventions. Front Allergy. 2023;4:1152927. doi: 10.3389/falgy.2023.1152927. https://pubmed.ncbi.nlm.nih.gov/36998574/
By Laurel Colless
CORP-RESP-1985
Orion Corporation is a globally operating Finnish pharmaceutical company. We develop, manufacture and market human and veterinary pharmaceuticals and active pharmaceutical ingredients. The dry powder inhaler developed at Orion is in the core of our respiratory therapy area.

