Dry powder inhalers – how to minimise handling errors and ensure patient satisfaction
Insights | 07/09/2022Prescribing information available here and Adverse event reporting information can be found at the bottom of this page.
Patient education in correct inhalation technique, handling, and storing of the inhaler is important to ensure successful inhalation therapy.
Levy et al. 2019 Adv Ther
- Poor adherence and incompetency in inhaler usage remain frequent problems with inhaled therapies for asthma and COPD.
- Patient education in correct inhalation technique, handling, and storing of the inhaler is important to ensure successful inhalation therapy.
- The patient should be involved in the selection of the inhaler in order to promote treatment adherence and satisfaction.
- From a patient’s perspective, a good inhaler can be defined by six E’s: the device should be effective, efficient, engaging, error-tolerant, easy-to-teach, and easy-to-switch to.
Modern inhalation therapy devices can be divided into four main types: the first devices resembled nebulizers and were introduced in 1860s, whereas metered dose inhalers (MDIs), dry powder inhalers (DPIs) and soft mist inhalers were developed in the 1950s, 1980s and in early 2000s, respectively. There is no single inhaler that would be an ideal option for all asthma and COPD patients, and the wide spectrum of devices with complex principles of action make the selection of an optimal therapy challenging. The main characteristics of different types of inhalers, including their benefits and disadvantages, are summarised in Table 1.
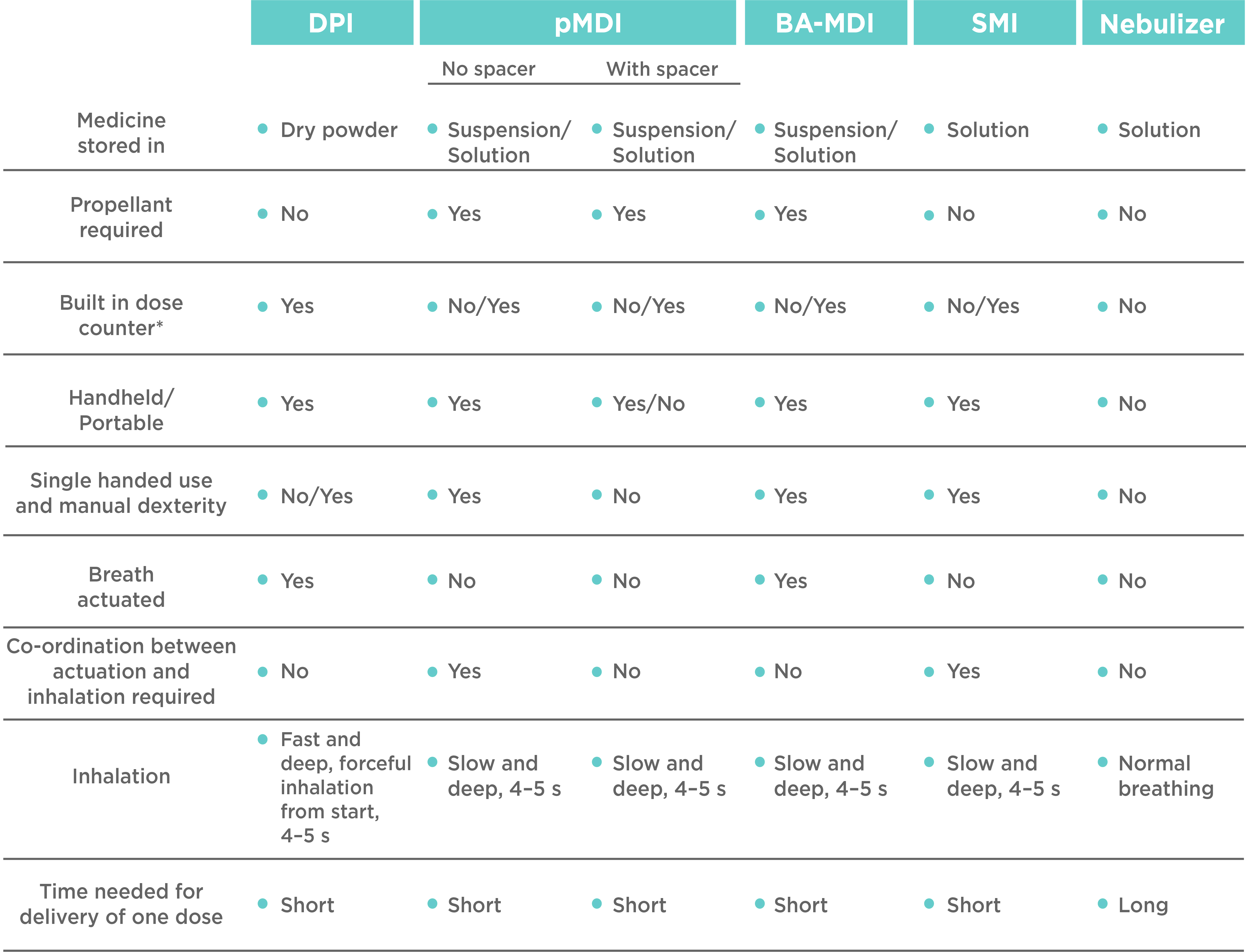
Table 1. Comparison of the benefits and disadvantages of different types of inhalers. DPI, dry powder inhaler; pMDI, pressurised metered dose inhaler; BA-MDI, breath-actuated MDI; SMI, soft mist inhaler. *Highly appreciated by patients, and thus increasingly included in inhaler devices.
An optimal therapeutic effect requires efficient delivery of the drug to the site of action. In pulmonary delivery, the selection of a suboptimal inhaler may limit the therapeutic efficacy of the drug. Despite the seemingly simple appearance, DPIs are sophisticated devices, and a compelling option for inhalation therapy due to their portability, ease of use and relatively low carbon footprint.
Studies suggest that the use of inhalers is not intuitive, and mistakes are common. With DPIs, the most common mistakes include exhaling into the device before or after the inhalation and lack of holding breath after the inhalation. While errors in inhaler use are known to affect the treatment outcome, direct comparisons between different inhalers are currently missing. To ensure efficient therapy, education of patients in the correct use of an inhaler is vital at the time of diagnosis, at regular intervals, and especially when switching inhalers. Environmental factors may also affect the function of DPIs. For this reason, training of the correct inhaler technique should also involve instructions in how to correctly store and handle the device. DPIs are very resistant to microbiological contamination, but humidity may affect the composition of the powder and thus the inhaler performance.
It has been shown that patient satisfaction with an inhaler is associated with adherence and disease control. From the patient’s perspective, the properties of an ideal inhaler can be summarised with six E’s that define an optimal inhaler as:
- Effective: delivers drug particles of the right size to the correct site of action with minimal adverse events irrespective of the inhalation flow rate.
- Efficient: is easy to handle, thus minimising handling errors and promoting compliance.
- Engaging: promotes patient satisfaction and adherence leading to improved treatment outcomes.
- Error-tolerant: minimises the effects of most common user errors.
- Easy-to-teach: is fast and simple for a physician to teach, to perform regular check-ups.
- Easy-to-switch to: is easy and efficient to switch t, if needed.
Current guidelines for asthma and COPD emphasise the involvement of the patient in the selection of an inhaler. While some of the usability aspects, such as size, portability and ease of use may appear trivial for the practitioners, they are known to be key features in patient satisfaction and may define the success of the treatment.
Bufomix (budesonide/formoterol) Easyhaler is the only Easyhaler preparation available in the Republic of Ireland.
Bufomix (Budesonide/Formoterol) Easyhaler Contraindications and Undesirable Effects
Contraindications:
Hypersensitivity to the active substances or lactose monohydrate (which contains small amounts of milk protein).
Undesirable effects:
Common (≥1/100 to < 1/10): Candida infections in the oropharynx, pneumonia (in COPD patients) headache, tremor, palpitations, mild irritation in the throat, coughing, dysphonia including hoarseness.
See SmPC for full list of adverse reactions
Reference:
Levy ML, Carroll W, Izquierdo Alonzo JL, Keller C, Lavorini F, Lehtimäki L. Understanding dry powder inhalers: key technical and patient preference attributes. Adv Ther 2019;36(10):2547–57.
Date of preparation: June 2024 / EASYH-2635(1)
| Adverse effects should be reported. You can report side effects directly via the Health Products Regulatory Authority (HPRA) website: www.hpra.ie or by email on medsafety@hpra.ie. Adverse effects should also be reported to Orion Pharma via ie.medicalinformation@orionpharma.com |




