Inadequate prescription, poor adherence, and errors in inhaler technique contribute to poor asthma control
Insights | 27/09/2022
Prescribing information available here and Adverse Event Reporting information can be found at the bottom of the page.
Inadequate prescription, poor treatment adherence and improper inhaler technique are some of the critical factors associated with poor asthma control,
Ribó et al. 2020 Prim. Care Respir. Med.
- Approximately two thirds of patients had poor asthma control at the primary care level.
- Critical factors associated with poor asthma control were inadequate prescription, poor treatment adherence, improper inhaler technique, and misconceptions about asthma.
- Of the 1,682 patients, 35.9% had an inadequate prescription, 76.8% showed low adherence and 17% exhibited mistakes with inhaler technique.
- Significantly fewer patients made critical errors with Easyhaler® than with other dry powder inhalers.
- The probability of poor asthma control increased when more risk factors were present.
Global increase in prevalence of asthma creates an economic burden for healthcare systems. Even with available therapies, asthma control appears suboptimal in primary care clinical practice. A cross-sectional multicentre observational study evaluated the proportion of asthma patients with inadequate treatment, poor treatment adherence, critical mistakes in the inhalation technique, and how these factors were related to poor asthma control. In total 1,682 adult patients with asthma who had been referred from primary care to a specialist for the first time were enrolled in the study.
Overall, according to Asthma Control Test (ACT) results, poor asthma control was found in 65.7% of the patients. The adequacy of prescription was evaluated according to the Global Initiative for Asthma (GINA) recommendations. More than one third (35.9%) of patients were found to have an inadequate prescription. Of these patients, 82.5% had poorly controlled asthma, whilst 56.3% of patients with adequate prescription had poorly controlled asthma (p < 0.0001). The maintenance inhalers used were multiple-or single-dose dry powder inhalers (DPIs) and pressurized metered-dose inhalers (pMDI), or some combination of both.
Approximately three out of four patients (76.8%) had low treatment adherence according to the Test of Adherence to Inhalers (TAI) questionnaire. Moreover, 68.8% of patients with poor adherence had poorly controlled asthma (according to the ACT), whereas 55.1% had poorly controlled asthma despite good adherence (OR 1.8, 95% CI: 1.42–2.27, p < 0.0001).
Errors with inhaler technique can affect treatment effectiveness. The study found that 17% of patients showed one or more critical errors, and 83.2% of these had poorly controlled asthma. In comparison, 62.1% of patients with no critical mistakes had poorly controlled asthma (p < 0.0001). When critical errors were compared between patients using different dry powder inhalers, significantly fewer patients made critical errors with Easyhaler® than with other DPIs (10.3% vs. 18.3%, p < 0.05) (Figure 1).
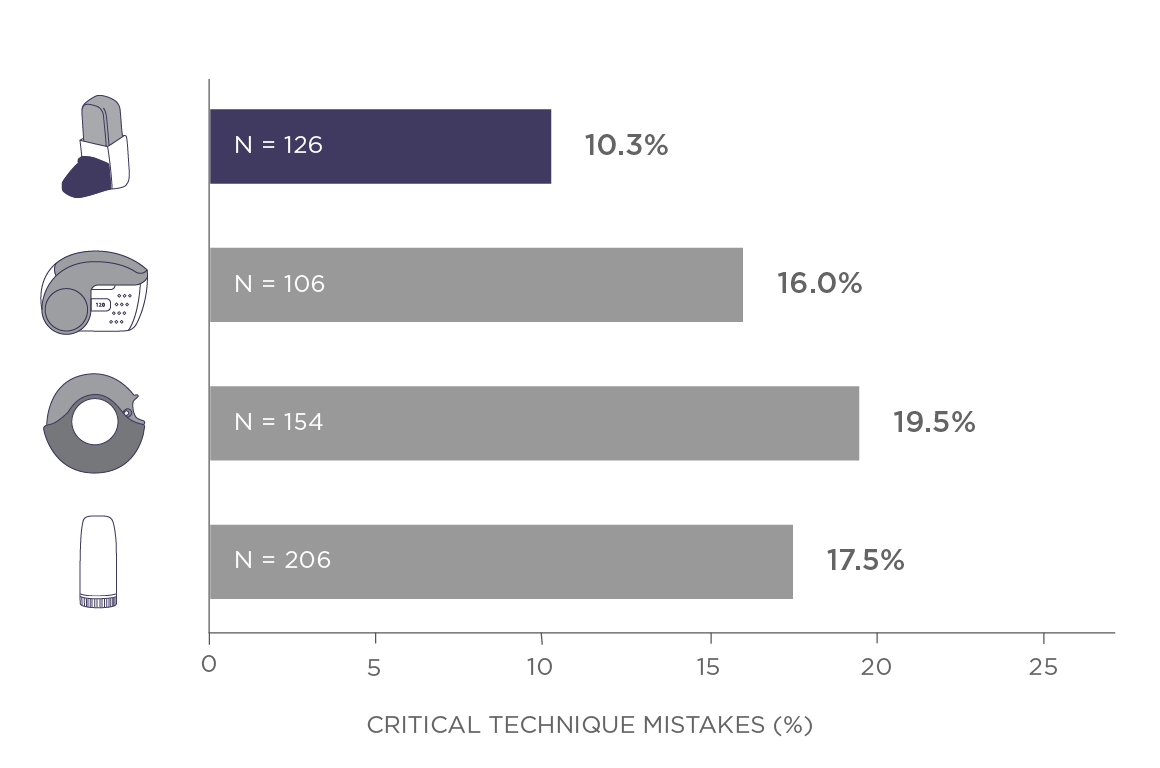
Figure 1. The proportion of patients who showed critical errors with inhaler technique, according to dry powder inhaler.
In addition, an asthma knowledge questionnaire revealed misconceptions about asthma treatment, as only 17.8% of patients were aware that bronchodilators are not the main asthma treatment and more than half believed they could stop taking anti-inflammatory treatment when they are asymptomatic. Poor asthma knowledge was found to be an independent predictor of poor asthma control.
In conclusion, poor asthma control was found to be common among asthma patients at the primary care level. Critical factors involved in poor asthma control were inadequate prescription, poor treatment adherence, and mistakes with inhaler technique, each increasing the probability of poor asthma control. Compared with other DPIs, fewer errors were made with Easyhaler®. Moreover, poor asthma knowledge was found to be an independent risk factor of poor asthma control. The study highlights the importance of routine assessments of asthma control and treatment adherence, treatment optimization, as well as training for inhaler technique and asthma knowledge.
Reference:
- Ribó, P., Molina, J., Calle, M. et al. Prevalence of modifiable factors limiting treatment efficacy of poorly controlled asthma patients: EFIMERA observational study. npj Prim. Care Respir. Med. 30, 33 (2020).
Date of preparation: July 2024 / EASYH-2700(1)
| Adverse effects should be reported. You can report side effects directly via the Health Products Regulatory Authority (HPRA) website: www.hpra.ie or by email on medsafety@hpra.ie. Adverse effects should also be reported to Orion Pharma via ie.medicalinformation@orionpharma.com |



